Browsing: Women Health

The page provides quick access to a list of common diseases, syndromes, health conditions, and other topics of health importance pertaining to women’s health. The list is organized alphabetically. Links are provided to respective diseases sections that serve as a comprehensive and ultimate guide about the disease or health condition.
A gynecological disorder involves damage or risk to any female reproduction organ, which includes the abdominal and pelvic area, i.e., ovaries, uterus, fallopian tubes, vagina, vulva and breasts. Some of these disorders can even affect the proper functioning of the reproductive system and may create difficulty during pregnancy or child birth.
Healthcare professionals believe that every woman may suffer from one or another type of gynecological condition at some point in their life. In the past few years, the incidence of few gynecological disorders has sternly increased such as endometriosis, uterine fibroids and breast cancer. They have not only affected adult women, but teenage girls also have shown high incidence of certain gynecological diseases.
From puberty till menopause, a woman’s reproductive organs are continuously changing due to sexual activity, pregnancy and aging. These changes occur due to variation in hormonal levels in the body. An injury or a disease can also affect your reproductive system, leading to a gynecological disorder.
Common gynecological disorders include dysmenorrhea, vulvodynia, chronic pelvic pain, breast cancer, polycystic ovary syndrome, endometriosis, uterine fibroids, vaginitis and menstrual cramps.
Empowering Your Health: How to Manage Menopause With Confidence
Menopause is a big phase in a woman’s life. It signals the end of menstrual cycles and it’s a time…
Pregnancy is exciting and beautiful, but it also comes with swollen ankles, backache, and days where putting on socks feels…
Women’s Health and Hormonal Treatments: What You Need to Know
Endocrine therapies have changed how females deal with pregnancy, period troubles and change‑of‑life signs. These medical approaches bring ease and…
The Checks To Consider In Your 20s If You’re Worried About Your Fertility
It’s normal to feel worried about your fertility, even in your 20s. Whether you’ve got a health condition, a family…
It usually starts with a little something. Maybe it’s a weird twinge in your lower back, or maybe your hips…
You’d think after round-the-clock feedings, diaper duty, and navigating a flood of new emotions, sleep would come easily. The same…
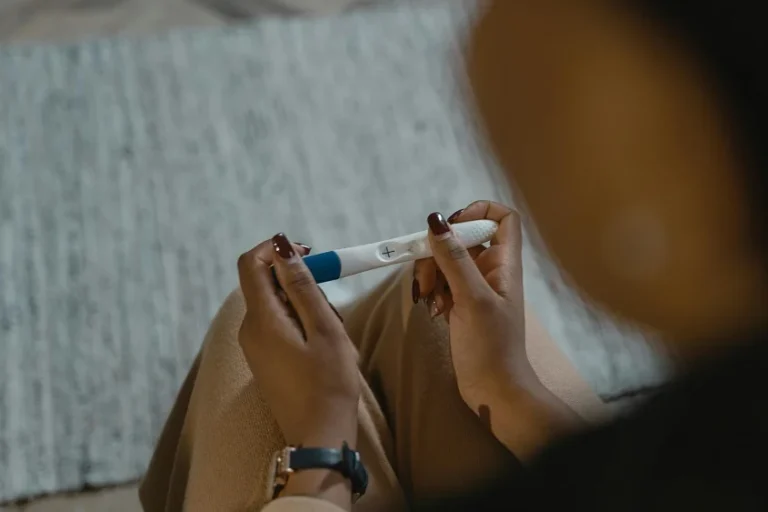
The Most Important Things To Think About After An Unexpected Pregnancy
You didn’t plan for this. One minute, life is moving along in its usual way—and then suddenly, there’s a positive…
Welcoming a baby into the world can be a delightful experience, but at the same time, it can also be…
Yeast Infections: What Causes Them and How to Prevent Them
Pexels. CCO Licensed. Yeast infections (also known as candidiasis) are a common type of fungal infection that most people will…
Proactive Steps to Reduce Miscarriage Risk: Proven Lifestyle and Medical Tips for Expecting Couples
Miscarriage is a heartbreaking experience for many couples, but there are proactive steps that can reduce the risk. Although it…