Tech Innovations Vs Working Conditions – What’s More Important to Improving US Healthcare?
- Updated on: Feb 10, 2025
- 2 min Read
- Published on Feb 10, 2024

The US healthcare system, well, it’s seen better days. You can’t open the politics page in the broadsheet without seeing a criticism of it. It costs too much and yet it doesn’t seem to have enough money. Physician staffing companies are dealing with constant strikes and staff members are dealing with worries about the effect of new tech, coming from everyone from hospitals to care homes.
So where would you allocate funds if the money was in your wallet? Much like plenty of other decisions made in healthcare, the ramifications are enormous. We’re breaking down the argument for whether tech or working conditions have more of an effect on healthcare. Read on for the details.
Pro-Tech Innovations:
In its broadest terms, healthcare can’t survive without innovations in technology. Even the basic scalpel had to be refined and reworked from the idea of a shiv to something fit for purpose. Nowadays we have everything from paperless patient charts and history to AI-assisted diagnosis and treatments.
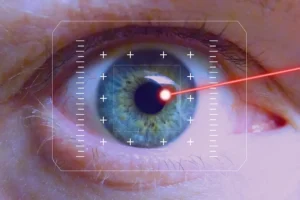
New technologies like AI, telehealth, remote monitoring devices, and robotics can improve efficiency, lower costs, and expand access to care. This directly benefits patients. Tech can streamline administrative tasks and allow healthcare workers to spend more quality time with patients. It is designed to augment some human capabilities but also improve some. Innovations like surgical robots and
Healthcare is lagging behind other industries in adopting new technologies, which is a shame considering how vital it is relative to other industries. Investing in innovation is key to modernizing the system, but so is access. Many small clinics and rural hospitals lack funds to invest in tech. However, government grants and incentives could accelerate adoption.
Pro-Improving Working Conditions:
Then again, no institution works without its staff, no matter what AI might be telling you right now. It’s important to have hard-working, intelligent, human staff because being in healthcare means handling peoples’ lives. That takes a careful touch and a steady hand – and often more soft skills than hard. Reform starts with workers. Empowering frontline staff to shape better workflows and processes drives innovation.
However, all of these soft skills are dampened by bad working conditions. For example, poor staff-to-patient ratios overburden healthcare teams and lead to mistakes, infections, readmissions. Burned out, overworked healthcare staff provide lower quality care. Improving working conditions improves retention and outcomes. Additionally, outdated EHR systems and complex admin tasks contribute to clinician burnout. Upgrades and automation would help.
Staff wellbeing influences patient experience. Investing in workplace wellness initiatives pays off in better care. The healthcare labor shortage and high turnover results from dissatisfaction. Better conditions are key to attracting talent.
Conclusion
Ultimately, this argument comes down to the people versus the supplies. And the unhelpful result for accountants to get their head around is that both are vital. How you divide up the budget comes down to the aspect that needs it most in your hospital, but that is a very nitty, gritty problem to tackle.
Review Process For This Article:
- Al-Antari MA. (2023). Artificial Intelligence for Medical Diagnostics-Existing and Future AI Technology.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9955430/